Achalasia is a rare, chronic disorder of the esophagus that affects its ability to move food toward the stomach. It occurs when the nerves of the esophagus and lower esophageal sphincter (LES) become damaged, causing a range of symptoms including difficulty swallowing (dysphagia), regurgitation, and chest pain. This condition is often confused with other digestive issues, which makes accurate diagnosis critical. Although there is no known cure for achalasia, several treatment options can help manage its symptoms and improve quality of life.
In this article, we will explore the causes, symptoms, diagnosis, and treatment options for achalasia, along with its potential complications and how it affects day-to-day living.
What is Achalasia?
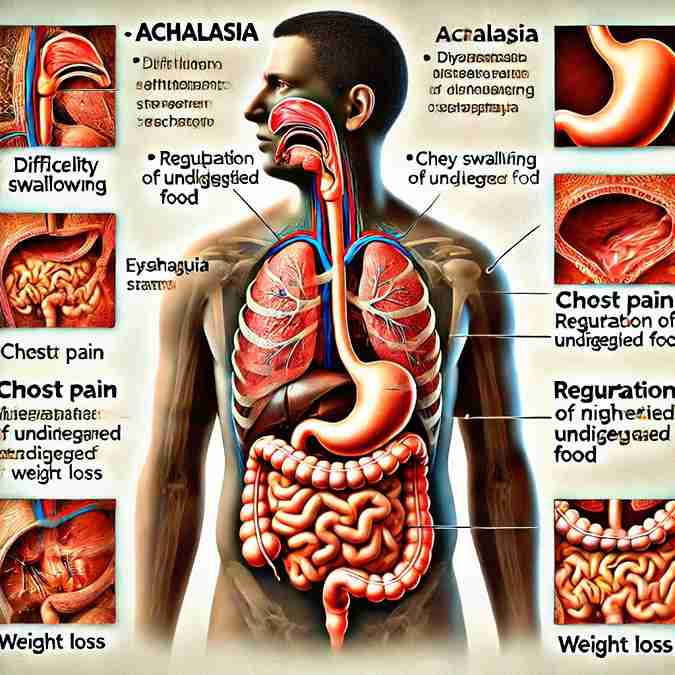
Achalasia is a disorder that impairs the normal peristalsis (muscular contractions) of the esophagus and affects the functioning of the LES. The esophagus, which is the muscular tube that connects the mouth to the stomach, relies on coordinated contractions to move food from the mouth to the stomach. In patients with achalasia, the LES fails to relax properly to allow food and liquids to enter the stomach, and the muscles of the esophagus lose their ability to contract effectively.
Causes of Achalasia
The exact cause of achalasia remains unknown, but it is believed to involve an autoimmune response that damages the nerve cells in the esophagus, specifically the myenteric plexus, which controls muscle contractions. This nerve damage prevents the LES from relaxing and impairs the peristaltic movements of the esophagus.
Several factors are thought to contribute to the development of achalasia:
- Autoimmune Response: Research suggests that achalasia may be triggered by an autoimmune response in which the body’s immune system attacks the nerve cells in the esophagus. This leads to the loss of nerve function and the disruption of normal esophageal motility.
- Genetic Factors: Some studies suggest a genetic predisposition to achalasia. While no specific gene has been identified, people with a family history of the disorder may be at increased risk.
- Viral Infections: Certain viral infections, such as herpes simplex virus (HSV) or Chagas disease (a tropical parasitic infection), have been linked to the development of achalasia. Chagas disease, in particular, is known to cause damage to the esophageal nerve cells, leading to symptoms similar to achalasia.
- Idiopathic: In many cases, the cause of achalasia remains idiopathic, meaning it has no identifiable cause. This is the most common form of the disorder.
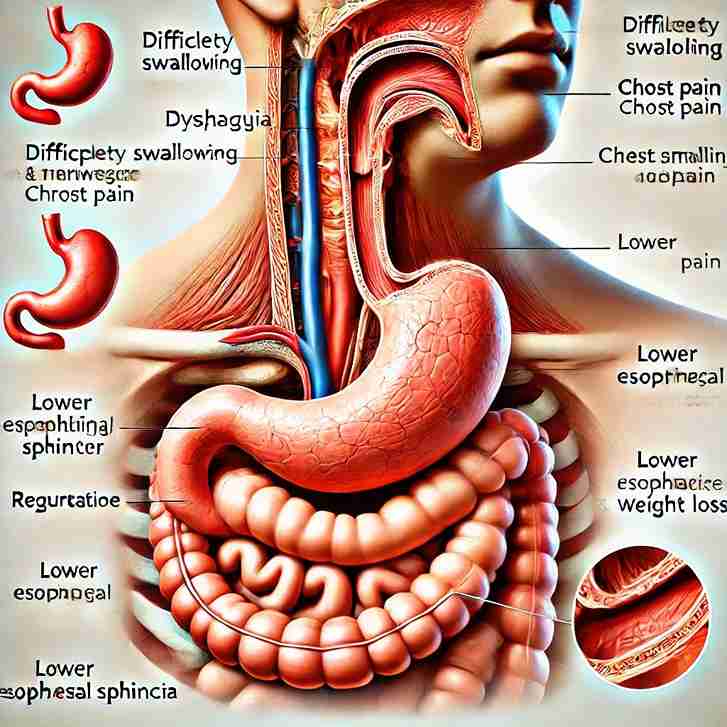
Symptoms of Achalasia
The symptoms of achalasia can vary from person to person, but the hallmark symptom is difficulty swallowing (dysphagia), which worsens over time. Other common symptoms include:
- Dysphagia (Difficulty Swallowing): People with achalasia often experience difficulty swallowing both solids and liquids. Initially, it may be most noticeable with solid foods, but as the condition progresses, even liquids may be hard to swallow.
- Regurgitation: Regurgitation of food, liquid, or saliva is a common symptom. This occurs because the LES does not relax properly, preventing the passage of food into the stomach. The food may return to the throat or mouth, sometimes leading to aspiration (food or liquid entering the lungs), which can cause coughing and choking.
- Chest Pain: Many individuals with achalasia experience chest pain or discomfort, which can mimic the pain of heart disease. The pain is often sharp or pressure-like and may occur after eating.
- Weight Loss: Difficulty swallowing and regurgitation can lead to unintentional weight loss due to reduced food intake and poor nutrition.
- Heartburn: Though achalasia is not typically associated with acid reflux, some individuals may experience symptoms similar to heartburn. However, this is not due to stomach acid, but rather a result of food or liquid being trapped in the esophagus.
- Coughing and Choking: As food or liquid regurgitates into the throat or mouth, it can lead to coughing, choking, or the sensation of food “sticking” in the chest.
Diagnosis of Achalasia
Diagnosing achalasia requires a combination of medical history, physical examination, and specialized tests. Early diagnosis is important to prevent complications such as malnutrition, dehydration, and aspiration pneumonia.
- Barium Swallow (Esophagram): This is often one of the first tests used to evaluate achalasia. The patient drinks a contrast liquid (barium), which allows X-rays to create detailed images of the esophagus. In patients with achalasia, the X-ray may show a “bird’s beak” appearance, where the lower esophagus narrows due to the failure of the LES to relax.
- Esophageal Manometry: This is the gold standard for diagnosing achalasia. During this test, a thin, flexible tube (catheter) is inserted into the esophagus to measure the pressure of the LES and the esophageal muscles. In achalasia, the LES pressure is abnormally high and does not relax, while peristalsis in the esophagus is either absent or severely impaired.
- Endoscopy: An endoscopy involves the insertion of a flexible tube with a camera (endoscope) through the mouth to visualize the inside of the esophagus. Although this test may not directly diagnose achalasia, it can help rule out other conditions such as cancer or strictures that could be causing the symptoms.
- High-Resolution Manometry (HRM): This advanced technique provides a more detailed assessment of esophageal motility and is particularly helpful in diagnosing subtle forms of achalasia and differentiating it from other esophageal disorders.
- Esophageal pH Monitoring: In cases where acid reflux is suspected, this test can be used to monitor the acid levels in the esophagus over a 24-hour period.
Treatment Options for Achalasia
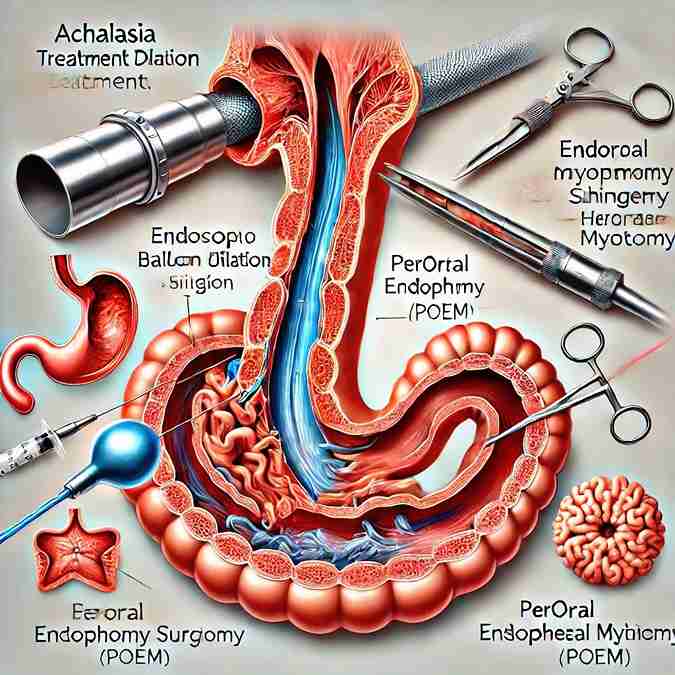
While there is no cure for achalasia, various treatments are available to help alleviate symptoms and improve esophageal function. Treatment aims to relieve the pressure at the LES, restore the normal function of the esophagus, and improve the passage of food into the stomach.
1. Medications
- Nitrates and Calcium Channel Blockers: These medications can help relax the LES, making it easier for food to pass into the stomach. However, their effectiveness is often limited and they are generally used as a short-term solution.
- Botulinum Toxin (Botox): Injections of botulinum toxin into the LES can temporarily relax the muscle and improve symptoms. This treatment may be useful for patients who are not candidates for surgery or other procedures, but its effects are often temporary and may wear off after several months.
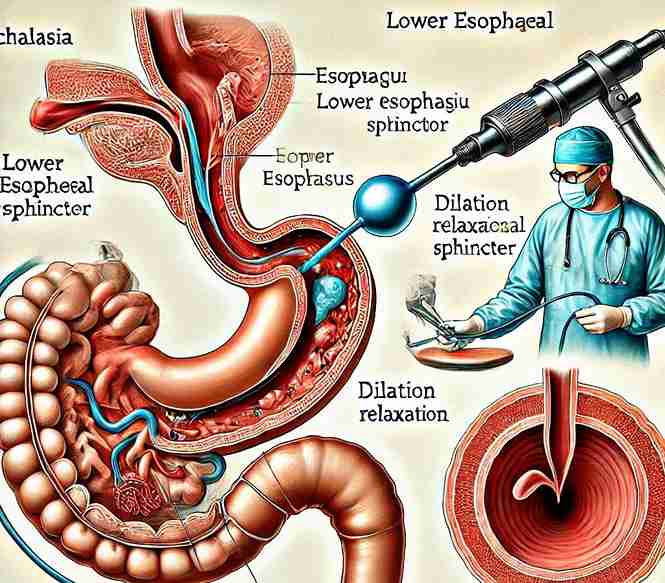
2. Pneumatic Dilation
Pneumatic dilation involves using a balloon to stretch the LES and break the muscle fibers that are causing the obstruction. The procedure is typically done under sedation and can be highly effective in relieving symptoms. However, it may need to be repeated over time, and there is a risk of perforation (a tear in the esophagus), though this is rare.
3. Surgical Myotomy (Heller Myotomy)
Surgical myotomy is considered one of the most effective long-term treatments for achalasia. During this procedure, the surgeon cuts the muscle fibers of the LES to relieve the obstruction. The procedure is typically performed laparoscopically (minimally invasive), meaning small incisions are made, and a camera is used to guide the surgery.
Heller myotomy has a high success rate, with most patients experiencing significant symptom relief. However, it may be followed by a procedure called fundoplication, which prevents gastroesophageal reflux (GERD) from occurring due to the loss of LES function after the myotomy.
4. Peroral Endoscopic Myotomy (POEM)
POEM is a newer, minimally invasive procedure that involves performing a myotomy through the esophagus using an endoscope. It has shown promising results in treating achalasia, particularly for patients with more severe forms of the disease. This technique is performed through the mouth, avoiding external incisions, and typically has a quicker recovery time compared to traditional surgery.
5. Dietary Modifications and Lifestyle Changes
While these are not a substitute for medical treatments, dietary changes can help patients manage their symptoms. Recommendations may include:
- Eating smaller, more frequent meals to reduce the amount of food in the esophagus at one time.
- Chewing food thoroughly to ease the swallowing process.
- Avoiding very dry, tough, or hard foods, which can be difficult to swallow.
- Drinking plenty of fluids with meals to help move food down the esophagus.
Additionally, patients may be advised to avoid lying down immediately after eating and to sleep with the head of the bed elevated to prevent regurgitation.
Potential Complications of Achalasia
If left untreated, achalasia can lead to several serious complications:
- Malnutrition and Weight Loss: Due to difficulty swallowing and regurgitation, individuals may struggle to consume enough nutrients.
- Aspiration Pneumonia: Food or liquid that regurgitates into the lungs can lead to infection, which may cause coughing, difficulty breathing, and fever.
- Esophageal Cancer: Chronic achalasia can increase the risk of esophageal cancer, especially after many years of disease. This is thought to be due to the inflammation and changes in the lining of the esophagus over time.
Conclusion
Achalasia is a complex disorder that can significantly impact a person’s quality of life. While the exact cause remains unclear, advances in diagnosis and treatment options have improved the management of this condition. Early detection and intervention are essential for preventing complications and maintaining a healthy, active lifestyle. Treatment options, including medications, pneumatic dilation, and surgery, offer a range of solutions to help patients manage symptoms and improve esophageal function.
If you or someone you know is experiencing symptoms of achalasia, such as difficulty swallowing, chest pain, or regurgitation, it is important to consult with a healthcare professional for a proper diagnosis and treatment plan.